
A pedestrian walks past a Christmas-themed graffiti depicting an angel, in Berlin, December 17, 2020. Photo: Reuters/Fabrizio Bensch.
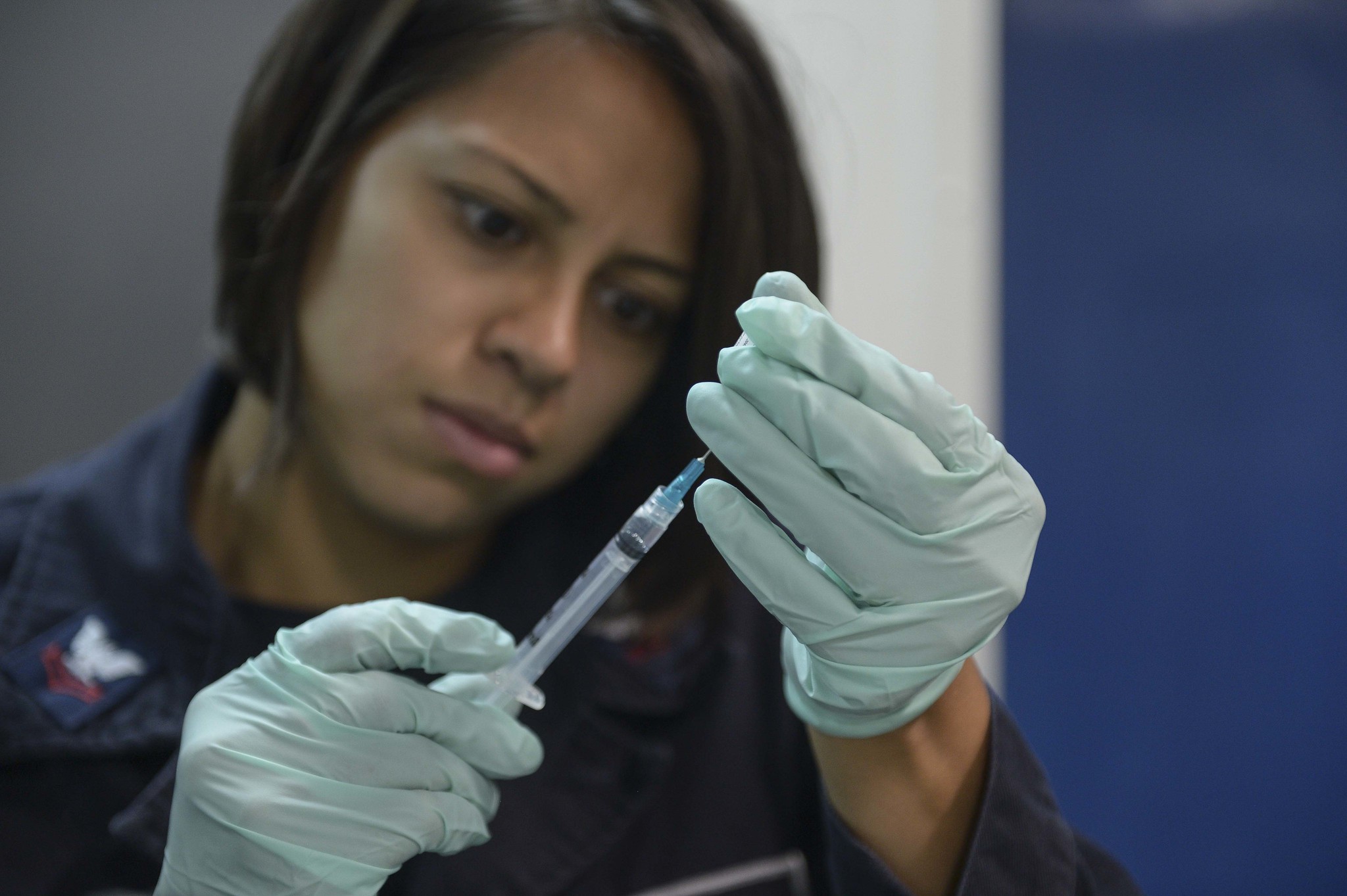
When nurse May Parsons administered the first injection in the world of the Pfizer-BioNTech COVID-19 vaccine to ninety-year-old British grandmother Margaret Keenan, applauded by dozens of moist-eyed medical staff at University Hospital Coventry, it was as glorious and moving a moment as any humanity has ever seen.
A jaw-dropping marvel of science, economic planning, and selfless, humanist cooperation by thousands of researchers around the globe, the development of this and other vaccines hot on Pfizer’s heels has taken a mere nine months since the discovery of the disease, rather than the years or even decades such medical research and development (R&D) normally takes. They offer a glimpse of how much more an egalitarian, rationalist world could produce and achieve, freed from the fetters of profit.
While the American private pharmaceutical giant and its German biotech start-up partner may bear the name of the first vaccine, this is no triumph for capitalism. Pfizer-BioNTech, along with the second-place finisher, Moderna, and the other front-runners, all depended on years of public-sector funding for their success, and, in many cases, on research actually performed by government or public university labs long before 2020. And again during this plague year, these private companies relied on state shepherding and bankrolling of the vaccine development process or, in the case of Pfizer, state-guaranteed purchase of millions of doses.
In many cases, national governments arranged purchase agreements and manufacturing support ahead of clinical trial results so that rollout could start as soon as regulatory approval was given, rather than having to wait for approval before manufacture could begin. Washington promised to purchase some $2 billion worth of the Pfizer vaccine and guaranteed about $2.5 billion to Moderna for the development and manufacture of its option.
The incredible speed of vaccine development just about makes up for the all-too-predictable news that the head of Pfizer cashed out 62% of his stock on the same day the company released the results of its vaccine trial showing 90%-plus efficacy, and that executives at Moderna made similar moves after their own announcement. In both cases, the stock sale occurred through what the firms insist was an entirely by the book, prearranged application of Rule 10b5-1, which insider trading law permits. But, as NPR has reported, experts in insider trading ethics say this is the thinnest of defences of what is “very suspicious” or even “wholly inappropriate” behaviour. Even if we are gullibly charitable in our assessment of the ethics of these moves, strategically, they remain profoundly stupid, given the scale of vaccine hesitancy.
It is not enough to be ethical; one must be seen to be ethical as well. So, to even appear to be engaging in insider trading with respect to vaccine development is a gift to anti-vaxx campaigners and COVID-19 conspiracists.
Such insider trading ethical fiascos aside, the rapid development of the vaccine has stunned experts. They knew more than anyone how long it normally takes for vaccine development. For years, these same infectious disease researchers, clinicians, and public health officials have damned the pharmaceutical giants for largely getting out of the business of vaccine development several decades ago. Contrary to anti-vaxx legend, pharmaceutical companies are, in reality, loath to engage in vaccine production because of the financial risk involved and their sheer unprofitability. Now, suddenly, in the face of a nigh-on existential threat, when the state bashes CEO heads together and takes on all financial risk, vaccines of stunning efficacy appear after just months.
It is almost identical to what happened during World War II, when the US government, frustrated with the intransigence of chemical companies and nascent pharmaceutical firms again fearing lack of profitability, simply ordered cooperation across enterprises, made investment decisions on behalf of the private sector, and covered the costs of research, development, and manufacturing. The result was the development or improvement of ten vaccines of military significance. The same wartime planning efforts produced the mass rollout of the first antibiotic, penicillin.
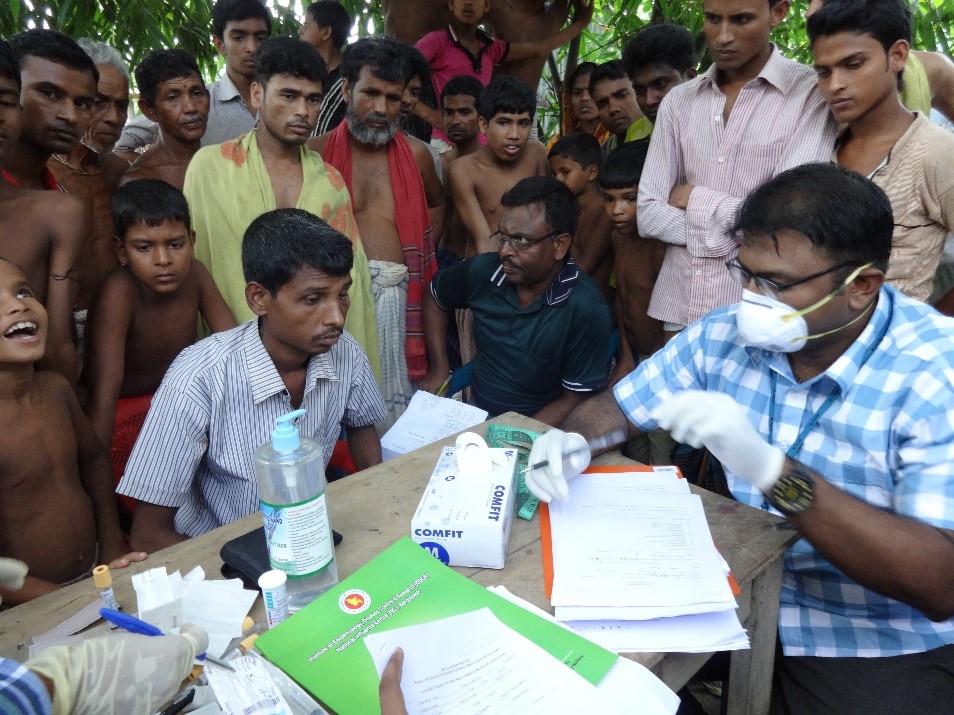
Moving forward, these lessons show that the inefficiencies of the market must now permanently be done away with for vaccine development related to all other infectious diseases that suffer from a dearth of private R&D. For tuberculosis (TB), for example, we have only a feeble, century-old vaccine that ameliorates the problem but is insufficient to prevent deaths from TB each year equivalent to those killed by COVID-19. In 2020, COVID-19 killed 1.7 million worldwide; in 2019, TB killed 1.4 million.
But before we get out the champagne and toast our genuinely heroic scientists and clinicians, we have to recognise that while these vaccines are indeed a light at the end of a very long tunnel, that same tunnel will be yet longer than it needs to be, thanks once again to the irrationality, inefficiency and injustice of capitalism.
It will be especially unfair for those in the developing world – and even in many poorer, less populous parts of the developed West, there will be cruelties for those who live outside the metropolitan core, as there already have been throughout 2020 in the United States especially. In the spring, stories abounded of testing, PPE, and ventilation machines being distributed on the basis of who could pay the most rather than who needed them the most. Even Republican governors of small states were fuming at how orders, paid in full, for essential equipment were canceled – sometimes mid-shipment – so as to make more money servicing richer jurisdictions. An almost identical crime is already in progress once again, but this time with respect to the logistics of vaccine manufacture and distribution.
mRNA revolution
To explain the profound injustice and hair-pulling inefficiencies of what is about to happen with respect to the domestic and worldwide distribution of the COVID-19 vaccines, we need to take a brief detour to explain how these vaccines work – in particular, how the ones first out of the gate are very different, even revolutionary, compared to other vaccines.
Conventional vaccines work essentially the same way they did upon their discovery in the days of Louis Pasteur. Inoculation involves exposure to a weakened or killed virus, which thus presents to the immune system an antigen – a molecular structure that is part of a pathogen that prompts an immune system response. The antigen we are focused on, with respect to the SARS-CoV-2 virus that causes COVID-19, is the infamous “spike” protein that covers its surface. The immune system then is able to remember and recognise any “live” version of the pathogen if, in the future, it attempts to invade the body. Now the immune system has a ready-prepared capability of combating and defeating it. Depending on the virus, this protection can last for life, a few years, or even a few months – hence the need for booster shots for some vaccines.
Traditional vaccines have been around for well over a century, and so the technology is mature and the manufacturing process is well established – even if the supply chain is somewhat withered due to the aforementioned decades-long retreat by Big Pharma from not just vaccine R&D but also vaccine production. The major challenge with respect to rapid rollout of traditional vaccines is that they need to be “grown” in hens’ eggs or insect cells. Each batch takes several weeks.
There are eight main vaccine techniques, including a handful of traditional, weakened virus versions, among the roughly two hundred candidate COVID-19 vaccines currently at various stages of development (there are fifty-seven presently undergoing clinical trials). Right now, the Pfizer-BioNTech and Moderna vaccines are of most immediate interest and are the most exciting in terms of the possibility that they may revolutionise vaccine production. They are messenger RNA, or mRNA, vaccines, the concept of which has been in development for many years – funded primarily by, you won’t be surprised to hear by now, the public sector. (The Oxford-AstraZeneca vaccine uses a different method, or “molecular platform” – more on this shortly.)
Messenger RNA, as you might remember from high school biology, is the molecule that transcribes the instructions in your DNA. This transcription is then read by ribosomes, the little machines in your cells that use these transcribed instructions to manufacture the proteins that make up almost everything in your body. With mRNA vaccines, instead of presenting the immune system with a whole virus, which has taken weeks to grow in hens’ eggs, just this bit of mRNA, embedded in a lipid nanoparticle (a fat molecule that helps it enter a cell) with the instructions on how to manufacture a viral antigen, is injected into the body. The mRNA then directs the cell’s ribosome protein factories to produce copies of the antigen (the spike, in this case), sans virus. The immune system recognises the spikes as foreign and attacks them, then subsequently remembers how to attack when confronted with the real thing.
It’s very clever on a number of levels. Far smaller doses are required to prompt an immune response, which means greater quantities can be produced much more rapidly than traditional vaccines. Also, once the genetic sequence for an antigen protein is known, you can quickly repurpose the same manufacturing equipment – bioreactors – for this new antigen. Conventional vaccine manufacture, meanwhile, requires slightly different bespoke equipment each time. The mRNA molecular platform had already been developed well ahead of the COVID-19 pandemic, which meant that as soon as the gene sequence for the spike was identified, which happened within days of the disease’s discovery, the vaccine could immediately start being produced. What took time was the clinical trials, and to speed them up, the different phases of the trials were performed in parallel instead of sequentially, as is normal practice.
This is the reason vaccine development has been so fast.
In the future, when confronted with other outbreaks of novel viruses, so long as we have set up the mRNA production equipment ahead of time, ready to go, we can simply fire them up with the new antigen genetic sequence. As it may be a long time between outbreaks, without any opportunity for profit, such facilities will likely need to be maintained or at least funded by the state simply as a public service, like sewage systems or, more analogously, like fire brigades, paid primarily to just be there, ready for when the emergency comes.
Ten-grand freezers and two-grand thermoses
The downside is that while some other types of vaccine can be kept stable in regular refrigerators, the lipid nanoparticle vehicles for the mRNA need to be kept ultracold to avoid breaking down. The mRNA molecule likewise begins to fall apart at room temperature. The Pfizer-BioNTech vaccine requires refrigerators that can keep the combo at a cozy -70º C.
And this, what is called a cold chain – a low-temperature-sensitive supply chain – is where we confront just the first in a series of hurdles to efficient and fair rollout of the vaccines that are caused by or exacerbated by market irrationality.Food distribution worldwide already depends on a highly developed cold chain, but an ultracold chain, with the sort of temperatures the Pfizer vaccine requires, is a step beyond that. It’s common for research labs to have freezers that can keep things that cold, but not the pharmacies where, for example, you might have received a flu shot.
Pfizer is shipping the vaccine in dry ice pack boxes. Once received, the dry ice needs to be replenished within a day. Once taken out of the dry ice pack boxes, the vaccine can be kept at regular refrigerator temperatures for twenty-four hours, or a maximum of two hours once thawed at room temperature. Ultracold freezers can extend shelf life by six months and are, in principle, commercially available.
As a result, major hospitals in metropolitan areas are running around trying to get their hands on these very cold but also very expensive freezers (which cost $10,000-15,000 a pop). And much like the hunt for personal protective equipment (PPE) and ventilation machines in the spring, a disorganised every-man-for-himself approach has returned in the winter. Rural areas and towns with smaller populations are being trampled in the stampede. The pandemic has bludgeoned the finances of less well-off hospitals, and these are expenditures they often just cannot afford. Even those hospitals that could afford one or two freezers are being told by manufacturers that delivery will take months; wealthier, larger hospitals that are able to buy in bulk get priority.
In an essential piece in the biomedical news service STAT on the scandal of flyover-state ultracold chain inequality, Olivia Goldhill quoted a director of sourcing for Vizient, a group purchaser for hospitals, as saying: “It’s another good example of how all our rural hospitals are at the end of a supply chain with less leverage to make important purchases. It’s the wild west of the supply chain; that’s not how you fight a pandemic.”
This is not merely unjust; it’s irrational. The regions and hospitals able to bid the highest are not necessarily the ones most in need. Rural areas and small towns tend to have a higher percentage of older people, as well as greater numbers of poorer residents, who, in turn, have a greater incidence of underlying conditions. This need-versus-supply mismatch then extends the length of the pandemic beyond what it might otherwise be, which endangers those wealthier regions more than necessary, because none of us is safe until all of us are safe.
And this is in the wealthiest country in the world. If ultracold chain management is beyond the reach of small-town America, the situation is even more dire in the developing world. In the least developed countries, the barrier is not merely access to the right sort of freezers, but reliable electricity to power any sort of refrigerator at all.
Ebola vaccines were able to be distributed to different sites in the Democratic Republic of the Congo during the height of that regional epidemic, using special high-tech Arktek thermoses that can maintain their contents at the required ultracold temperatures. But the thermoses cost $2,000 each. Bill Gates is on the case here, promising to pick up the tab for Arktek thermoses for COVID-19 vaccines in regions like this. But humanity shouldn’t have to depend on the goodwill of billionaires to deal with a pandemic.

Other vaccines coming down the pipeline are less demanding. Moderna’s, with a similar efficacy to that of Pfizer, can be stored at just -20º C – within the temperature range of a regular freezer.
The hope is that other vaccine candidates using different approaches will be less temperature-sensitive. The vaccine developed by University of Oxford researchers who subsequently partnered with the British-Swedish pharmaceutical firm AstraZeneca also employs a novel molecular platform, this time a “viral vector” – an adenovirus that causes colds in chimpanzees but not in humans, whose genes are modified to produce the COVID-19 spike protein on its shell – but it can be stored at ordinary refrigerator temperatures. The Novavax vaccine, whose phase 3 clinical trials are due for completion at the end of January, is likewise fridge-stable, as is the vaccine developed by the Sanofi-GlaxoSmithKline partnership (although its results so far have been disappointing, and a reformulation of the vaccine means that approval likely won’t be given before the fourth quarter of 2021).
But under these circumstances, once again, in the developing world, or even in a US territory like Puerto Rico, which suffered from extended blackouts in the wake of Hurricane Maria, a plain old fridge is no use if the electricity cuts out for hours or days on end.
And what if the efficacy for these more easily distributable vaccine options is lower than the mRNA vaccines? The Oxford-AstraZeneca vaccine results initially suggest it is between 70% and 90% effective (compared to 95% for both Pfizer’s and Moderna’s options). This is still outstanding, and far superior to the 40-60% efficacy rates of the annual flu shot. But those in rural America and the developing world are still likely to feel that they are somehow second class, which, of course, from the market viewpoint, they are. And again, this is irrational, even for the rich: the mismatch between need and supply, delivering potentially less effective vaccines not to those in less need but instead to those with less wealth, unnecessarily extends the lifetime of the pandemic that threatens us all.
Vaccine priority access
Even if all the vaccine options had no issues with temperature sensitivity, other issues relating to production and distribution would be challenging enough. Given the reproduction rate (the infamous basic reproduction number, or R0) of COVID-19 observed in countries prior to lockdown, and assuming a vaccine with 100% efficacy, some 60-70% of the global population would need to be vaccinated in order to achieve herd immunity that will block SARS-CoV-2 transmission. The COVID-19 vaccines are not 100% effective, so the real number will be higher, but this gives us a good baseline for what needs to be achieved.
Both the Pfizer and Moderna vaccines are 50% effective after one dose and only achieve their higher efficacy rates with two doses. That would mean that, at a minimum, a total of over 8 billion doses needs to be manufactured to cover 60% of the world’s 7 billion people. For comparison, over the past decade, 1 billion children worldwide have been vaccinated against the likes of mumps, measles, rubella, polio, tetanus and yellow fever. This is why there is great hope being placed on the Johnson & Johnson single-dose vaccine.
Meanwhile, Pfizer predicts it will be able to produce 1.3 billion doses by the end of 2021. Moderna claims it can produce another billion in the same time frame. But does that work out to be roughly 2 billion? Not necessarily. A firm will be making these estimates based on what their own suppliers – of bioreactors, filtration devices, vials, nucleotides, enzymes and other inputs and equipment – estimate they can provide. The supplier will tell Pfizer they can offer 1 billion widgets, for example, but then Moderna will call the same supplier and get the same hypothetical number. Those 1 billion available widgets are for both of them combined.
Meanwhile, we are already seeing examples of brazen attempts at cutting in line. The doctor who is bribed by a wealthy patient to, nudge nudge, wink wink, categorise him as asthmatic is, however grotesque, not so much the problem. Numerically, these frauds shouldn’t amount to much. And the stricter the controls on such cheats, the greater the likelihood of increasing bureaucratic barriers to rollout. To some extent, one has to simply accept a certain level of selfish but petty villainy. It is the more wholesale corporate queue-jumping, lubricated by existing structures of professional lobbying, that threatens to push aside those in most urgent need of vaccination.
Even if everything ran smoothly from manufacture to local distribution, at the point of care – the site of actually injecting the vaccine into people’s arms – there are insufficient workers on the ground in the United States to perform the inoculation, as well as handling the associated advertising to explain where and how to get a shot (and to combat vaccine hesitancy), software programming and allied tasks. The Association of State and Territorial Health Officials and the Association of Immunisation Managers have requested that Congress deliver just over $8 billion to cover the cost at state level of recruiting and training extra staff. Some $200 million distributed to them from the CDC is all they have so far received.

In the spring, Hollywood studios spent hundreds of thousands of dollars successfully lobbying for essential worker classification in California, and World Wrestling Entertainment did the same in Florida. Today, as the first vaccines are released, the American Bankers Association is lobbying the CDC to have bank tellers and loan officers prioritised for vaccination as “essential workers,” as is the National Hockey League for its players, and Uber and DoorDash for its drivers.
Wild West, indeed. What is required is for government to step in to a greater degree than experienced under Donald Trump to plan, or at least shepherd with a firm hand, parts of the vaccine production and distribution supply chain, as occurred in the spring in many countries with respect to PPE, ventilators and hospital-bed manufacturing. The greater the flow of vaccine manufacture and distribution, the less such line-cutting matters.
Supply chain specialists argue that in the case of COVID-19, demand planning is of such a different magnitude compared to historic distribution of vaccines that it will require governments to normalise (stabilise) and optimise vaccine supply chains, just as was necessary with PPE. While President Trump eventually invoked the Defence Production Act (DPA) to force companies to produce PPE and used emergency use authorisations to permit new PPE suppliers to enter the market, for the most part, private markets were left to their own devices with respect to the PPE crisis, with insufficient government shepherding – and they largely failed.
A suspicious PPE “broker” market cropped up, wherein shady figures claiming to be brokers said they would help locate and acquire such equipment for hospitals, clinics, and other frontline organisations. While some of these were legitimate, if exploitative of a crisis situation, many were simply fly-by-night operations with no experience in medical supply chains. Either way, legitimate or criminal, the brokers regularly failed to secure what they had promised.
To prevent this from occurring again, Joe Biden could use a more aggressive application of the DPA, which permits the executive to incentivise firms to expand production within existing domestic manufacturing capacity of critical inputs to the vaccine supply chain, to incentivise expansion of new manufacturing capacity, and to employ people with the experience necessary to supervise and plan such production. Under the act, the federal government could commandeer the resources required, including requisitioning supply chain and logistics experts and suppliers to build a centralised procurement and delivery process. Should there be transport bottlenecks or shortages, the DPA also allows activation of the Civil Reserve Air Fleet – in essence, drafting private airlines like Delta or United.
It is inefficient for each of the states to design and put in place their own distinct vaccine distribution plans. Instead, the federal government is best positioned to organise information gathering across the entirety of the system, in assistance with local and state governments and health providers, and then to feed such data back down the chain in order to alter production and distribution plans as consumption of vaccines dynamically changes. It is precisely because the logistics are so complicated that the state needs to take over from the chaos of the market.
Vaccinationalism
But an aggressive swerve by the incoming Biden administration would only smooth out domestic supply chain crunches and market irrationalities. It would do nothing to arrest global vaccine injustice and illogic. In June, Jacobin reported how pharmaceutical firms such as Gilead Sciences, AstraZeneca and Sanofi were seeking extensions to their patents on drugs with potential COVID-19 applications, such as remdesivir (whose price Gilead jacked up to $3,000 per patient, even though the cost is just $9), and simultaneously lobbying to have language removed from a WHO resolution that referenced the right of countries to override patents during health emergencies in order to cheaply and quickly manufacture generic versions of the same drugs. The lobbying effort was in turn supported by US, UK, Japanese and Swiss diplomats.
Most of these same villains are at it again, but this time with respect to vaccines. Wealthy countries are attempting to block a proposal at the World Trade Organisation by South Africa and India to release member countries from requirements to enforce COVID-19-related vaccine patents.

Hilariously, the argument put forward by the US trade representative as to why is that a loss of such intellectual property protections, even temporarily, would threaten incentives for vaccine innovation – as if almost every penny of the cost of research, development, and manufacture of the vaccines did not come from the public sector. COVID-19 vaccine innovation is entirely a product of the state.
But regardless of the sheer audacity of these shameless bandits, the retention of a monopoly on COVID-19 drugs and vaccines necessarily restricts the supply. Again, the interest of these firms inhibits rational production and allocation. The objective function of human society right now is to defeat the virus as quickly as possible. It is at odds with the objective function of market actors: maximisation of profit. Even the rich that stand to profit from such patent enforcement are enhancing their own risk of being infected and dying from COVID-19 through this very initiative.
It is not surprising then, in this every-man-for-himself ethical environment, that in recent days, researchers at Duke University’s Global Health Innovation Centre have calculated that a handful of rich countries have already snapped up, through advance purchase agreements intended for domestic recipients, some 600 million doses of the Pfizer vaccine – almost half the amount that the company estimates it can produce by the end of next year. The study concluded that doses sufficient to cover just 250 million people have been purchased by COVAX, a global platform to guarantee equal access to COVID-19 vaccines regardless of a nation’s ability to pay. The COVAX pact aims to deliver some 2 billion vaccine doses by the end of next year, covering 20% of people in 91 countries in Africa, Asia, and Latin America.
Many of these rich countries that have signed side deals to ensure their domestic access to large vaccine shipments also signed up to COVAX. The pact was itself an initiative of France and the European Union. Yet these same countries are, in effect, undermining the very pact they signed by bidding their way to the front of the line. The researchers estimate that as a result of this “vaccinationalism,” most people in low-income countries will have to wait until sometime in 2024 to be vaccinated. Vaccinationalism will extend the pandemic by years. Making matters even worse, internal documents from the COVAX secretariat leaked to The Guardian have revealed that its managers believe the plan is at “very high” risk of failure, as it has only managed to raise $2.1 billion out of the $4.9 billion it estimates is necessary to meet its 20% by 2021 goal.
The best that humanity can hope for in the immediate term to defeat this vaccinationalism and the Wild West of vaccine rollout is popular, internationalist shaming of its injustice and irrationality. But looking beyond the horizon of COVID-19, the threat of future pandemics – and among them will be ones nowhere near as forgiving as this coronavirus – requires at some point a serious discussion of how global democracy can be constructed from the bottom up, and how in such a democracy, worldwide economic planning can tame the inefficiencies, irrationalities and injustices of markets.
What all this tells us is that economic planning in service of the speediest eradication of the disease is insufficient if such planning remains at the national level. In this case, each country is acting in the same self-interest as any Pfizer or Moderna CEO, but in the marketplace of national competition. Of course, COVAX was supposed to be that very supranational, extra-market superintendent of such global planning. But COVAX is not a global state. It has, like the WHO, neither sufficient resources nor the legal capacity to enforce its plan the way that a state does.
Because no one is safe until we are all safe.
Leigh Phillips is a science writer and EU affairs journalist. He is the author of Austerity Ecology & the Collapse-Porn Addicts. This article was first published by Jacobin and has been republished here with permission.

