
- Is molnupiravir as potent as its name suggests? It is so named to evoke the power of Mjölnir, the hammer of Thor.
- Merck’s investigational oral drug has generated much enthusiasm and has been hailed variously as a “breakthrough drug” and a “game changer”.
- But there is reason to believe that we don’t know all we can about the drug’s safety and that its real-world effectiveness may be lower than its tested efficacy.
The SARS-CoV-2 pandemic continues to ravage the world, with one-half yet to receive the first vaccine dose. Global efforts to combat the pandemic are being hampered by vaccine shortages, vaccine hesitancy and the emergence of new variants.
Many experts have said that eliminating SARS-CoV-2 is an unrealistic goal and that it may become endemic, continuing to persist indefinitely, in many countries. This would likely pave the way for the rise of new vaccine-resistant variants.
In this scenario, a safe, effective and affordable antiviral drug for the treatment of COVID-19, the disease caused by a SARS-CoV-2 infection, and for curbing the spread of the virus would be an invaluable tool. Antiviral drugs for COVID-19 have so far not been as promising as the vaccines. The only such drug to date, with modest benefit to COVID-19 patients, is Gilead’s injectable drug remdesivir. This drug is approved by the US Food and Drug Administration (FDA) but not by the WHO.
In these circumstances, Merck’s investigational oral drug molnupiravir, recently claimed to cut the risk of hospitalisation in COVID-19 patients by half, in phase 3 trials, has generated much enthusiasm and has been hailed variously as a “breakthrough drug” and a “game changer”.
The enthusiasm stems mainly from the fact that molnupiravir is a take-at-home drug, and the hope that it may be useful to people with weak immune systems, who may not benefit from vaccination.
Is Merck’s experimental drug as potent as its name suggests? (‘Molnupiravir’ is so named to evoke the power of Mjölnir[footnote]Pronounced myal-neer[/footnote], the hammer of Thor.) Let’s look at the available information, including the not so readily visible fine print, on molnupiravir.
What is molnupiravir?

Molnupiravir belongs to a class of broad spectrum antiviral drugs called nucleoside analogues. They act by interfering with the function of viral RNA polymerases – which are enzymes that make new viral RNA in infected cells.
Molnupiravir, initially called EIDD-2801, was invented by scientists at Emory University as a drug for the influenza virus. It is known as a pro-drug, as it must undergo conversion to its drug form first – a product called N4-hydroxycytidine (NHC) – before exerting its antiviral effect.
Prior to the advent of the current pandemic, NHC was shown to be a potent inhibitor of several other unrelated RNA viruses, such as the Ebola virus, the Venezuelan equine encephalitis virus and coronaviruses. In early 2020, NHC was shown to be effective against SARS-CoV-2 as well.
A small Florida-based pharmaceutical company, Ridgeback Biotherapeutics, acquired EIDD-2801 from Emory University in March 2020 and sold it to Merck two months later, and today partners with Merck, in what is being seen as an unconventional, even controversial, manoeuvre.
Molnupiravir the trickster

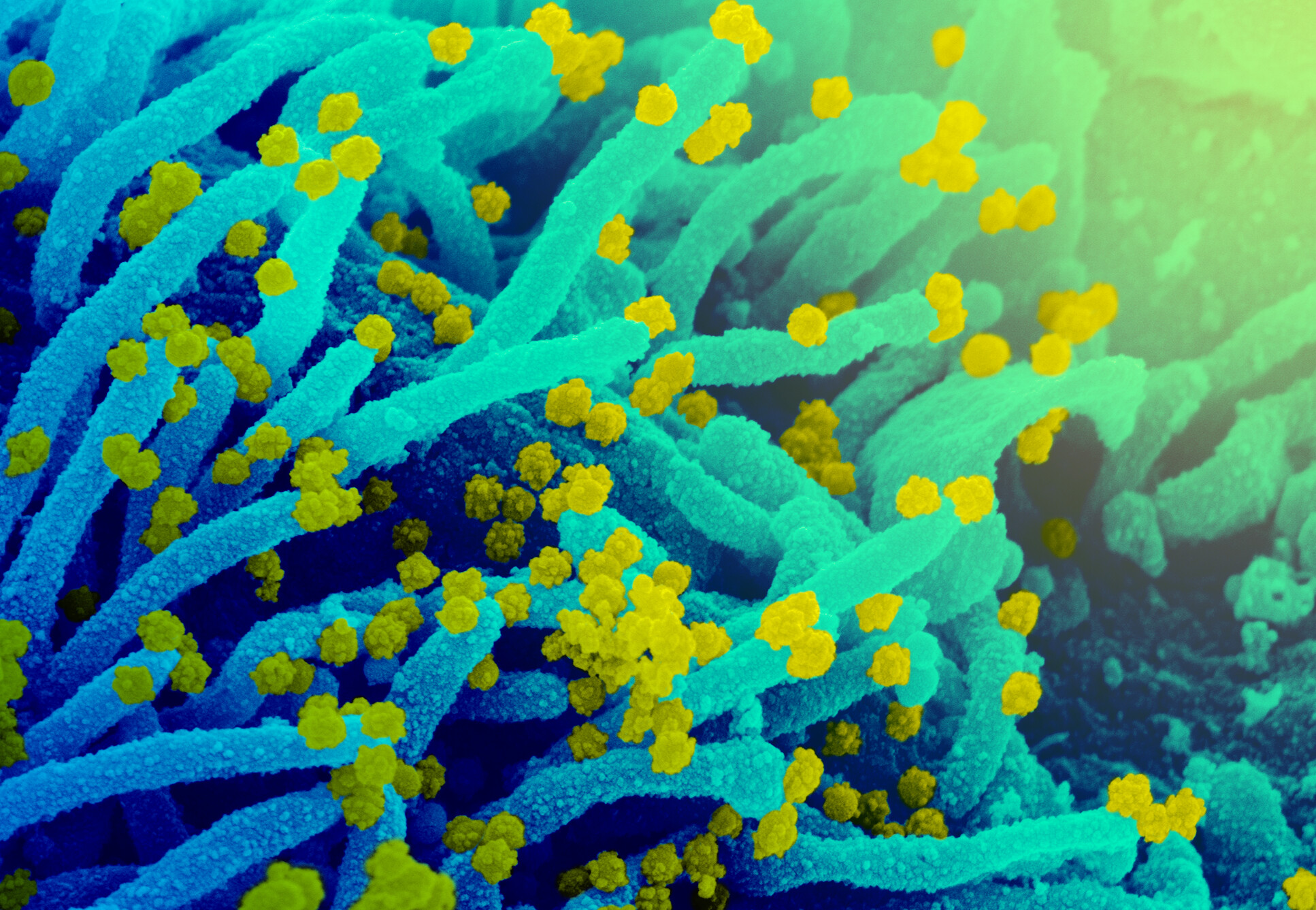
The genetic information required for the novel coronavirus to infect susceptible cells and produce millions of progeny viruses is encoded by a chemical substance called ribonucleic acid, or RNA. SARS-CoV-2’s RNA is a very long polymeric molecule containing four kinds of repeating chemical units – designated by the letters A, G, C and U. There are approximately 30,000 letters in the virus’s RNA, arranged in a particular sequence.
When the virus infects a cell, the genetic information in the viral RNA is decoded to make a set of specialised molecules called proteins. Each of these proteins performs a specific function, needed to successfully complete the virus’s life cycle in the infected cell, culminating in the release of millions of progeny viruses.
One important protein that is the target of molnupiravir is the coronavirus (CoV) polymerase. The specific function of the CoV polymerase is to make new copies of the 30,000 letter long SARS-CoV-2 RNA from the original viral RNA, introduced into the cell during infection. This process is called RNA replication. These new RNA copies are required so they can be inserted into the progeny viruses.
Using the original virus RNA as a reference – or template – the CoV polymerase strings together the four letters A, G, C and U in the same sequence. Newly synthesised RNAs serve as templates for further viral RNA synthesis.
Once in a while, the CoV polymerase can make a mistake and insert a wrong letter, much like a typo, into the sequence. When this happens, another viral protein called ExoN corrects the mistake: it removes the wrong letter, allowing the CoV polymerase to insert the right letter.
This self-correction is not perfect. Sometimes, mistakes may go unnoticed, resulting in a letter change known as a mutation. The function of ExoN is to keep mutations below a certain threshold. Above this threshold, the virus will not be viable.
Molnupiravir, rather its drug form NHC, is a look-like of the RNA component C (of the A, G, C, U). When it is present in an infected cell, the CoV polymerase can mistake it for a C and insert it into the new RNA molecule at positions normally meant for C. Unfortunately for the virus, ExoN ignores this mistake – because NHC inhibits it.
The result is new RNA molecules that are ‘tainted’. The CoV polymerase that can’t distinguish between the ‘tainted’ RNA template and the untainted version uses it as a reference to make more copies of new RNA, which are also tainted.
There is an additional problem for the virus, stemming from a unique chemical property of NHC that allows it to exist in two forms – by shifting the position of a specific hydrogen atom in its structure. This phenomenon is known in chemistry as tautomerism. This ends up confusing the CoV polymerase into additional wrong letters into newly synthesised RNA.
After several rounds of replication, the new viral RNAs end up accumulating mutations way beyond the threshold of viability. The genetic information in the viral RNA becomes so garbled that it can no longer direct successful virus multiplication. In effect, molnupiravir exerts its antiviral action against SARS-CoV-2 by lethal mutagenesis.
The actual details of the mechanism of action of molnupiravir on SARS-CoV-2 RNA replication were worked out in detail by two groups who published their findings in July and August earlier this year.
While all this provides a clue to how molnupiravir works against the novel coronavirus, we still need to ask how good molnupiravir would be as treatment for COVID-19. The announcement of interim data from Merck’s ongoing phase 3 trials has fueled hopes of a new tool to help curb the pandemic’s spread.
Merck’s trial

Merck initiated a phase 3 clinical trial of molnupiravir, dubbed ‘MOVe-OUT’, in non-hospitalised COVID-19 patients a year ago. Volunteers with COVID-19 were enrolled within five days of onset of illness, to ensure their infections were either mild or moderate. COVID-19 was confirmed based on laboratory testing.
The trial was designed to include only those patients who were regarded as being ‘at risk’ of progressing to severe COVID-19 and with at least one risk factor (such as diabetes, heart disease, obesity, older than 60 years, etc.) linked to poor disease outcomes.
Half of these volunteers were given 10 oral doses of molnupiravir, at 800 mg per dose, at 12 hour intervals over five days. The other half were given similar-looking oral capsules that didn’t contain molnupiravir. They were all monitored for 29 days after the first dose. This trial is slated to be completed by May 2022.
On October 1 this year, when data for over 750 patients had been collected, Merck announced that molnupiravir reduced the risk of hospitalisation or death significantly in these patients based on an interim analysis of the data. The efficacy of molnupiravir was pegged at 50%.
At the time of this analysis, 53 of 377 participants (14.1%) in the placebo group developed severe COVID-19 requiring hospitalisation, and eight of them died. In the molnupiravir-treated group, 28 of 385 participants (7.3%) progressed to severe disease requiring hospitalisation, and no one died.
This means molnupiravir reduced the baseline risk of severe disease and hospitalisation due to COVID-19 in at-risk patients from 14.1% to 7.3%. This is how Merck arrived at the 50% efficacy figure.
Note that 50% efficacy is synonymous with 50% inefficacy as well. Adverse events were comparable between the two groups. Merck also reported that analysis of viral sequences from a subset of patients indicated that molnupiravir was effective against viral variants gamma, delta and mu.
Merck stopped recruiting more volunteers for this study after the interim findings, characterised the results as compelling and expressed great optimism that molnupiravir could become an important tool with which to fight the pandemic.
It’s also notable that about a week after Merck’s claim on the efficacy of molnupiravir, two Indian drug-makers sought to end their own efficacy trials of the same drug – because the drug didn’t show any benefits in patients with moderate COVID-19. Merck explained this discrepancy as being due to differences in the way Merck and the Indian companies defined “moderate COVID-19”.
After withdrawing from its COVID-19 vaccine initiatives, Merck is moving rapidly to consolidate its position in the drugs arena. On October 11 – 10 days after announcing its interim results – Merck applied to the US Food and Drug Administration (FDA) seeking emergency-use authorisation (EUA) for molnupiravir, for the treatment of mild-to-moderate COVID-19 in at-risk adults. Three days later the FDA announced that it would convene a meeting on November 30 to examine Merck’s application.
Merck is also working on submitting similar applications to national drug regulatory agencies around the world. The European Medicines Agency has also started a rolling review.
Anticipating more positive results from its MOVe-OUT trial, and approval from drug regulators, Merck has also started producing the drug and expects to have about 10 million doses by the end of this year. It has signed a supply agreement for 1.7 million doses with the US government at $70 per dose, as well as deals with Singapore and Australia. Merck has also entered into non-exclusive voluntary licensing agreements with several Indian drug manufacturers (Cipla, Dr Reddy’s, Emcure, Hetero and Sun).
Is there a downside?

The most obvious downside to any drug would be possible safety risks due to unexpected side effects. Such effects arise typically due to the drug affecting parts of the body in addition to those that it should.
Molnupiravir is apparently designed to hit the virus and not affect the bodies of the people who take the drug. That is, it should be safe. But in the absence of conclusive evidence, it is hard to assert that molnupiravir will be absolutely safe.
The only information available is Merck’s statement on a safety follow-up for 29 days after the first dose. According to this, both the treatment and placebo groups in the phase 3 trial experienced similar and mild side effects, at similar rates. Will there be long-term effects? Merck suggests that they will be highly unlikely.
The antiviral effect of molnupiravir is linked to its capacity to induce mutational errors in the genetic program of the novel coronavirus. Our genetic code is encrypted in deoxyribonucleic acid (DNA), another long polymeric molecule, built of four kinds of building blocks (A, G, C, T versus the viral RNA’s A, G, C, U). In fact, in our body, RNA is converted to DNA in order to make new DNA.
This raises a very important question: could molnupiravir induce mutational errors in DNA? There are indications that this possibility shouldn’t be dismissed without due diligence.
Substances that can cause DNA damage, either through mutations or other means, are called genotoxins. There are two potential outcomes from exposure to a genotoxic substance, depending on the type of our body’s cells that may be affected. If normal cells undergo DNA damage, it could lead to cancer. If reproductive cells (sperms and eggs) suffer DNA damage, it could lead to birth defects in newborn babies.
In May 2020, a Science News report mentioned possible safety issues linked to molnupiravir, flagged by a US government scientist. This scientist’s concern was based on the fact that molnupiravir belongs to a class of compounds known to cause serious birth defects in animal experiments. The same article reported that an Emory University scientist had found that Pharmasset Inc., acquired by Gilead Sciences in 2011, abandoned the development of a drug similar to molnupiravir in early development, due its mutagenic properties, many years ago.
In January this year, another US scientist raised the possibility that molnupiravir could be potentially mutagenic to DNA and lead to cancer. Within our cells, DNA is present not only in the cell nucleus but also within another component, called the mitochondria, whose function is necessary for powering all life activities. Drugs belonging to the class of nucleoside inhibitors, of which molnupiravir is a member, are known to be toxic to mitochondrial DNA. This means we certainly need to know if molnupiravir can damage DNA in mitochondria as well.
However, Merck announced on April 15 this year that it had carried out specific tests in animals to examine the drug’s potential to cause DNA mutations. According to Merck, the totality of its data indicated that molnupiravir is neither mutagenic or genotoxic. Merck reiterated this in a recent publication writing that it did not consider molnupiravir to pose an increased risk of genotoxicity in clinical use.
It is still not clear if Merck carried out experiments with pregnant animals to rule out possible birth defects or if it determined mitochondrial toxicity.
A team of scientists from the University of North Carolina actually examined if NHC could indeed cause mutations in DNA, in a study published in August this year. They used a test to identify DNA mutations in a gene called HPRT in laboratory cultured animal cells. The function of this gene makes the cells susceptible to being killed by a drug called 6-thioguanine (6-TG).
The scientists worked on the hypothesis that if the cells are cultured in the presence of NHC, and if NHC induced mutations in the HPRT gene, it could lead to the gene becoming non-functional. This in turn would lead to the cells becoming resistant to 6-TG.
They found that cultured cells indeed acquired resistance to 6-TG upon NHC exposure. They also found that the HPRT gene of these cells had acquired new mutations. In a nutshell, NHC could induce mutations in the DNA. What we need to know now is how efficient the process by which NHC may be converted to a DNA building block look-alike is. Would this cross into the nucleus and mitochondria to inflict DNA damage?
Merck disagreed strongly with this study, citing the same animal experiments it invoked on April 15. The university scientists have in turn argued that Merck’s attempt to justify the safety risk as ‘non-existent’ based on negative data is untenable. It is also telling that Merck’s molnupiravir phase 2a and phase 3 trial volunteers were required to agree either to observe strict sexual abstinence or to use highly effective contraceptive methods during the trials, and for a certain period after the trial itself. Men were also required to refrain from donating sperm.
Merck’s abundant caution – despite its assertion on molnupiravir’s safety profile – could have been to preclude pregnancies during the trial as they could potentially result in birth defect(s). It’s hard to believe then that Merck itself believes that the mutation risk to individuals taking molnupiravir is zero. It ensured zero risk in its trials; that is not possible in the real world.
Resistance to molnupiravir
The expectation that molnupiravir could be an effective tool to fight the pandemic could be rendered meaningless if the novel coronavirus develops resistance to it. Can this happen?
Molnupiravir acts by increasing the frequency of mutations in the viral RNA – by inhibiting ExoN. Based on this, one could imagine a situation in which the viral RNA encoding ExoN may suffer a set of mutations that make it insensitive to the drug, while at the same time retaining its ability to correct occasional errors made by the CoV polymerase. If so, this would skew the drug’s risk-benefit ratio.
At this time, we don’t have many drugs that can inhibit the novel coronavirus, and we know practically nothing about mutations that can give it the power of drug resistance.
There is one piece of scientific investigation, published in late 2019, before the pandemic struck, that examined the emergence of resistance to NHC (the drug form of molnupiravir) in coronaviruses. This report concluded that low-level resistance to NHC could be seen in the viruses after prolonged exposure. These drug-resistant viruses had acquired several mutations. Scientists call the minimum number of mutations required to acquire resistance to a drug the genetic barrier. NHC has a high genetic barrier to the emergence of drug resistance.
In real-life situations, will this barrier be high enough? We still don’t know a lot about SARS-CoV-2 to be able to produce definitive answers.
Molnupiravir v. hype

In sum, is molnupiravir the “game changer” it has been hailed as? The answer is not a definitive ‘yes’ – since at this time the interim data is not conclusive. Data from just under 400 patients in each group has been analysed and is yet to be made publicly available. The available safety data is definitely preliminary. Merck, or independent researchers, need to show rigorously that a drug designed to damage viral RNA will not damage the patients’ DNA, in the cell nucleus or in the mitochondria.
We also don’t know of potential long-term safety issues. Not knowing of or lack of evidence about safety issues at present doesn’t mean that such risks are either ruled out or non-existent. Some – if not many – of us may recall the tragedy of birth defects linked to the use of the drug thalidomide in the 1950s and 1960s.
The optimism for molnupiravir needs to be tempered with caution. That it has 50% efficacy also means that it has 50% inefficacy against COVID-19. The 50% efficacy achieved in preventing progression to severe disease is possible only if the drug is taken very early after disease onset. While this can be strictly implemented in a clinical trial, it is unlikely to happen in real life. This then means real-world effectiveness could possibly be lower.
The cost of a full course of molnupiravir, amounting to $700 (Rs 52,450), could be a limiting factor as well, especially in resource-poor countries (and if Merck sells it at the same price). Effective deployment of the drug – once it is proven to be adequately safe – will depend on the availability of diagnostic tests, increasing the total cost of the treatment.
Finally, despite Merck’s efforts to lower the drug’s price in resource-poor countries, molnupiravir’s utility could be limited by wealthier nations trying to stockpile it, as they have done with COVID-19 vaccines as well.
Ultimately, molnupiravir will have to be a lot cheaper and more safe if it is to have a meaningful impact on the pandemic. We need to regard this drug with caution, not hype. The FDA is expected to grant Merck the EUA it has sought for molnupiravir, perhaps by this year’s end – and not for all, but only certain groups of people.
S. Swaminathan is a retired scientist based in Hyderabad. The views expressed here are the author’s own.

