
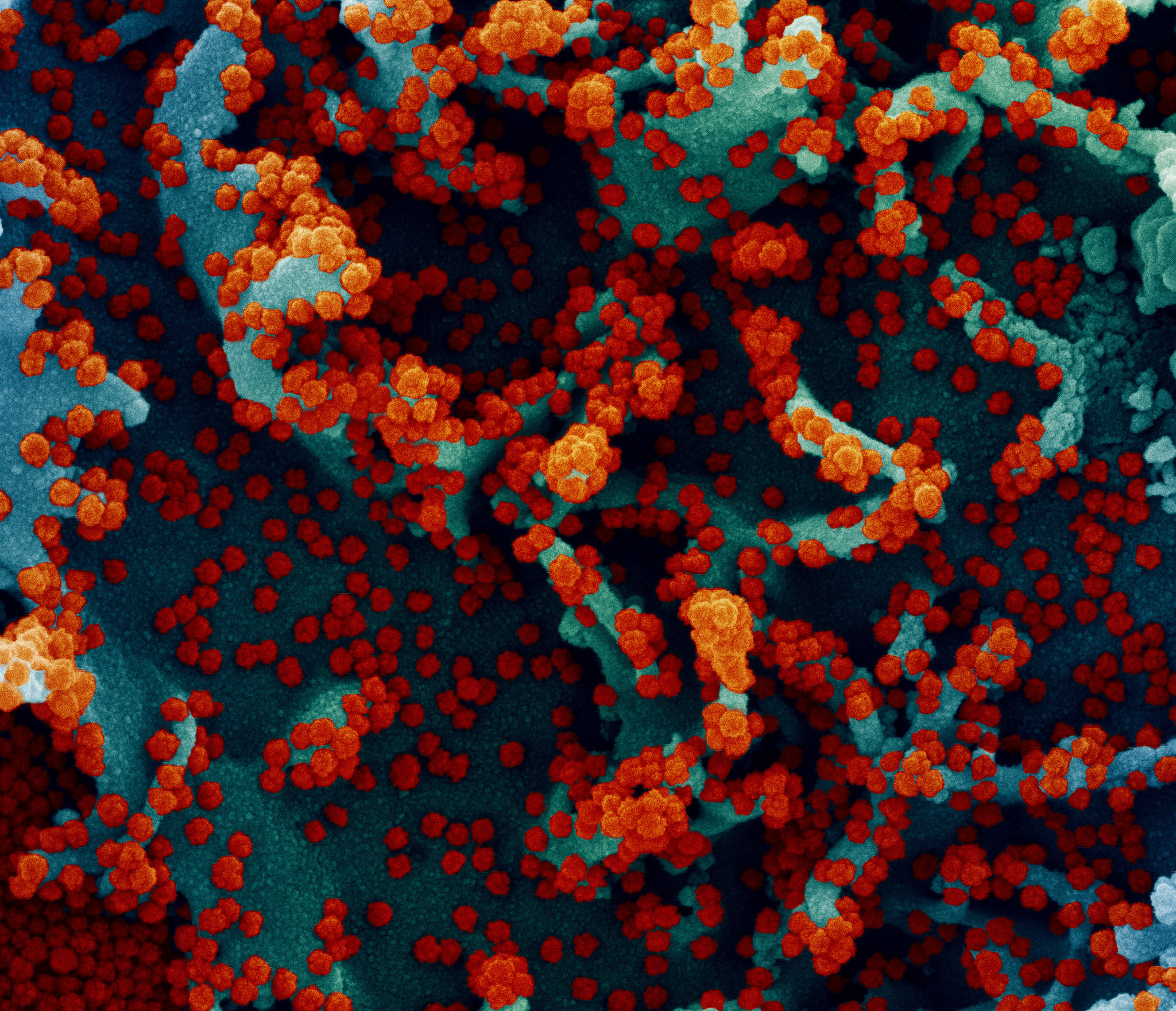
Illustration: ColiN00B/pixabay.
Bengaluru: Rakesh Mishra, the director of Hyderabad’s Centre for Cellular and Molecular Biology (CCMB), is frustrated. CCMB has been sequencing SARS-CoV-2 viral genomes since the COVID-19 pandemic began – initially as part of its own research program and since December 2020 as part of the Indian SARS-CoV-2 Genomics Consortium (INSACOG), a group of ten labs the government put together to ramp up sequencing across to India.
To do its work, Mishra’s team needs specialised plastic containers and reagents that go into sequencing machines. But buying them has become needlessly complicated in the last year, taking time away from his lab’s core jobs, according to Mishra.
The source of his troubles is a finance ministry order in May 2020 that stopped government labs from importing goods worth less than Rs 200 crore. The order was meant to boost local manufacturing, in the spirit of ‘Make in India’, but had unintended consequences for India’s fledgling genome-sequencing efforts. Several reagents and plastics used by Indian labs come from foreign manufacturers, like the US-based Illumina Incorporation, and have no Indian substitutes.
The ministry’s sudden restrictions threw these labs out of gear. By September 2020, sequencing across the country had come to a near-complete halt, as labs ran out of reagents they needed. Then, in response to their complaints, the ministry exempted reagents from its restrictions in January 2021.
But plastics are now the new thorn in his side, Mishra said. These materials still haven’t been exempted from the ministry’s order, which means his lab can’t buy them in bulk unless it can conduct a market assessment to show that no Indian alternatives exist. Such an assessment is a needless bureaucratic distraction at a time when labs desperately need to sequence more viral genomes – and faster. “It’s like asking us to run a 100-metre dash with our hands tied,” Mishra said. “I can run, but I will run very slow.”
Ill-timed government orders are just one hurdle that INSACOG labs have had to cross to sequence genomes faster across India. To pull this off, these labs need several stars to align: COVID-19 testing labs must preserve positive samples from patients, state governments must transport these samples to the ten INSACOG labs every week, and the labs must be able to buy the equipment they need to sequence quickly.
None of this has been happening two months since INSACOG was launched. To begin with, the Rs 100 crore fund that INSACOG had requested from the Union science ministry hasn’t arrived yet. Without the money, most labs can’t buy the equipment they need, and are progressing slowly with their own funds.
“We are excited to be part of INSACOG, but the money needs to come, otherwise how can we ramp up?” Uma Ramakrishnan, a molecular ecologist at the National Centre for Biological Sciences (NCBS), Bengaluru, which is part of the consortium, asked. Others say that even if labs could sequence more, states aren’t yet sending them enough samples. The reasons range from a lack of coordination between state governments and INSACOG labs to restricted availability of the right kind of RT-PCR samples needed for sequencing.
If INSACOG had followed its implementation strategy to the letter, it ought to have sequenced 5% of all positive cases in India since November 23, in addition to samples from international travellers. This adds up to at least 80,000 sequences by now. Instead, as on February 24, 2021, the consortium had completed only 3,500 sequences. And unfortunately, the labs with the most capacity, including CCMB and the Institute of Genomics and Integrative Biology (IGIB) in New Delhi, have remained heavily under-utilised.
While IGIB can sequence up to 10,000 samples a month, it has only received over a third of this number from Punjab, Haryana, Rajasthan, Kerala and Uttar Pradesh combined, said Anurag Agarwal, the institute’s director. Meanwhile, CCMB, which can sequence 5,000 samples a month, has received fewer than 200 samples from Telangana, Andhra Pradesh and Northern Karnataka, which are the areas in its purview.
Three ambitious goals

For all the obstacles it faces, INSACOG’s work has never been more crucial.
Since the novel coronavirus pandemic began, several new variants of the virus have shown up worldwide. Among them are B.1.1.7, a highly contagious variant first reported from the UK, the B.1.351, a variant that first emerged in South Africa and is known to diminish the efficacy of some vaccines, and B.1.1.28, a variant from Brazil. Large outbreaks in Maharashtra and Kerala today have raised the question of whether genetic changes in the virus could be driving them.
To pick up such changes as they emerge in the viral population, and to stop them from spreading elsewhere, the government needs a coordinated and continuous surveillance program like INSACOG, said Vinod Scaria, a genomics researcher at IGIB.
Yet, until December 2020, India didn’t have such a programme. Instead, a few labs were working on their own steam to map how SARS-CoV-2 was evolving. They either used samples that came to them for testing or tied up with state governments interested in mapping the virus’s evolution. As a result, sequencing was both meagre and spotty for a country India’s size: labs got their samples from a few interested states like Kerala, Gujarat and Andhra Pradesh, but large parts of the country were flying under the radar.
In November, fears of the B.1.1.7 variant spreading through the country swung the government into action. It launched INSACOG, led by the National Centres of Disease Control (NCDC) in New Delhi. Nine other labs, including the National Institute of Virology (NIV), Pune; the National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru; NCBS, CCMB and IGIB will cover all states between them. The idea was that the NCDC would co-opt its deeply entrenched network – the Integrated Disease Surveillance Programme (IDSP) – to liaise with state governments and route samples from them to the ten labs.
The consortium has three ambitious goals. The first is to map the spread of the B.1.1.7 variant across India. The second is to investigate regional outbreaks, by collecting samples from multiple times from these regions so that new variants, if any, can be intercepted. The third is to set up a continuous surveillance program to sequence 5% of all samples across the country every month – in line with what countries like the UK have been doing.
Trouble finding old samples

As of today, work has begun only on the first and second goals, and both have also quickly run into hurdles. To determine if B.1.1.7 was in India – a goal later expanded to B.1.351 and B.1.1.28 as well – INSACOG was supposed to sequence samples from every international passenger who tested positive for COVID-19 since November 23, 2020, and from 5% of all positive cases across India between November 23 and December 22. That is, as soon as INSACOG was kicked off in December, states ought to have dug into their archives, found old samples from passengers and the general populace, and dispatched them to the labs.
This didn’t really happen.
International-passenger samples were easy to collect, but states struggled to locate old samples from 5% of all cases since November 23, NCDC director Sujeet Kumar Singh said. There were many reasons. First, many of the positive samples had been tested using antigen tests, and few labs stored these samples after the test was done. Second, finding old samples from even RT-PCR tests [footnote]A test to detect viral nucleic acids in the sample by amplifying them several times[/footnote] has been an uphill task. Testing labs are required to store these samples at a temperature between -80º C and -20º C, and labs across the country are not required to do this beyond a month, given freezer-space constraints.
A third hurdle is that sequencing works best for samples that have a high viral load or with an RT-PCR cycle threshold [footnote] Cycle threshold is a measure of the viral load, Lower threshold means higher viral load.[/footnote] of less than 25. “So to find B.1.1.7, we focused only on RT-PCR samples which were available with labs, and which had low cycle threshold,” said Singh.
These restrictions shrunk the pool available for sequencing to a minuscule fraction of the intended 5% (45,000 out of 9,35,251 of positive cases), according to Singh. Eventually, a total of 3,500 sequences were completed by February, of which INSACOG had detected 187 instances of B.1.1.7, four of B.1.351 and one of B.1.1.28. And of these, the B.1.1.7 variant had been detected in 18 states, among both international travellers and people who’d had no contact with such travellers.
Singh said this data meets INSACOG’s first goal because it shows that the B.1.1.7 variant is spreading in the community within India. And now that this has been established, there’s good reason to stop looking at old samples because the task has been painstaking and cost-intensive. “We have submitted to the health ministry that the first goal of INSACOG is fulfilled. Once it is done, we don’t see a rationale in pursuing it further,” he said.
Other scientists in the consortium agree. If one, some or all of the three variants are behind local outbreaks, sequencing under INSACOG’s second and third goals would pick them up anyway, they said.
The problem is that progress on the second and third goals is also happening at a crawl.
Ramping up during an outbreak
The INSACOG consortium’s second goal is to investigate outbreaks like the ones ongoing in Maharashtra and Kerala. For this, scientists typically sequence samples from people in the outbreak area at multiple time points, over weeks. If a particular variant seems to be spreading faster than others, the next step would be to figure out if it has an evolutionary advantage. B.1.1.7, for example, has mutations that allow it to bind to human cells better, which in turn makes it more transmissible. (See box: Are the E484K and N440K variants worrying?)
After COVID-19 cases spiked in Maharashtra in late January 2021, the B.J. Medical College, Pune, reportedly identified the so-called E484K mutation in one patient sample from the Amravati district and the N440K mutation in a sample from Yavatmal. The findings sparked speculation that these mutations may be behind Maharashtra’s climbing cases. Scientists have previously found in lab studies that these genetic changes can help the virus evade some human antibody responses. Clinical trials found the performance of the Novavax and Johnson & Johnson vaccines to be reduced in South Africa, which has a high prevalence of the E484K variant.
Does this mean E484K and N440K are something to worry about? It’s too early to say. Establishing this would require a large number of samples to be sequenced from Maharashtra. By all accounts, B.J. Medical College has sequenced only a handful.
Meanwhile, INSACOG hasn’t begun sequencing the samples it asked the affected districts to send (see main story). Once it sequences samples across several weeks in Maharashtra, and if this data shows a large and growing fraction of E484K or N440K infections, that would suggest that these mutations have some evolutionary advantage – such as an increased ability to transmit or to reinfect previously sick people.
N440K is not new – it has been on Indian scientists’ radar for a while. The last time it attracted attention was when scientists at CCMB spotted it in 34% of samples they sequenced from Andhra Pradesh in August and September 2020. Because the mutation seemed to be widespread then, it was important to track its spread across India, said Divya Tej Sowpati, a scientist at CCMB. But these efforts were thwarted by a change in India’s import rules (see main story), freezing most sequencing efforts across the country. N440K then fell off the radar for a while, according to Sowpati.
There is some in vitro evidence that N440K can dodge parts of the human immune system. In one study, published in October, US researchers found that in the presence of a monoclonal antibody called C135, which is also being investigated as a drug for COVID-19, a recombinant version of the SARS-CoV-2 virus quickly acquired the N440K mutation to evade the antibody. And of the handful of cases of COVID-19 reinfection in India that scientists have sequenced thus far, N440K was present in one.
Still, this is far from strong evidence that N440K causes reinfections. The way a virus behaves in a lab doesn’t always translate to how it behaves in an epidemic. Also, even if a mutation may help a virus evade a monoclonal antibody, people may still be able to fight off the virus with other antibodies and components of their immune system, such as T-cells.
Additionally the fact that N440K was so common in Andhra Pradesh without causing any noticeable increase in reinfection cases suggests it may not be so concerning, said Anurag Agarwal, director of the Institute of Genomic and Integrative Biology, New Delhi. Vinod Scaria’s work with sequencing samples from the outbreak in Kerala has also shown N440K to be present in 10% of the samples in some districts.
This is why INSACOG’s ongoing work in Maharashtra and Scaria’s group’s work in Kerala is crucial. By observing whether these mutations are becoming more frequent over time, they will be able to determine if the mutations had anything to do with the surges. Eventually, they may find that neither mutation has any role to play – or that a combination of both does. Or they may find an entirely different combination of mutations altogether.
A final distinct possibility, said Scaria, is that it’s not the viral genomic code that has changed in a meaningful way but the behaviour of people in affected states. If susceptible people who were not infected in Kerala’s or Maharashtra’s previous outbreaks stopped taking precautions, or began organising large gatherings, that could suffice to explain a lot.
But answering the question of whether the Maharashtra outbreak is being driven by new variants is not going to be easy. INSACOG has only now begun collecting samples from the 11 worst-affected districts, including Amravati and Yavatmal. Singh said the NCDC has asked these districts to send 100 samples each, obtained after January 23, when cases began growing exponentially. These samples are currently being transported to the two INSACOG labs handling Maharashtra samples: NIV and the National Centre for Cell Science, both in Pune. Once the samples arrive, researchers at these facilities may need up to two months to sequence and analyse the data.
But according to CCMB’s Mishra, this effort may not be enough. Instead of a one-time set of 100 samples from each district, the goal should be to sequence 100 samples each week, he said. “If a variant is beginning to emerge in these districts, it has to be followed up over several weeks,” he explained. Indeed, even INSACOG’s guidelines call for sequencing 5% of all positive samples every week in outbreak regions – which adds up to over 600 samples in February in Amravati. As of now, for reasons that are unclear, the NCDC has not instructed the districts to send more samples.
Kerala, on the other hand, has had a head-start in its outbreak investigations, thanks to a state-funded sequencing programme separate from INSACOG. Under this programme, the state tied up with the IGIB to send 25 samples from each of its 14 districts every week, starting from the last week December. Soon, IGIB will have a ten-week series of samples from Kerala, Scaria said, which will help his team decide if any new variants could be driving the state’s outbreak.
This said, even Kerala isn’t sequencing 5% of its positive samples yet. A state official who didn’t wish to be named told The Wire Science that this would happen only after INSACOG kicked off.
Continuous surveillance

The last and most difficult goal of INSACOG is the continuous surveillance programme – for which 5% of all positive samples must be sequenced continuously from every single state, instead of waiting for outbreaks to occur first.
This process has barely begun as labs wait for funds and states drag their feet on sending samples. While IGIB has received only 3,500 samples since November 23, CCMB has received fewer than 200.
The situation in other labs is no different. Ravi Vasanthapuram, a virologist with NIMHANS Bengaluru, another INSACOG lab, said his team had only sequenced 163 samples since November. Murali Dharan Bashyam, a molecular oncologist at the Centre for DNA Fingerprinting, Hyderabad, said they had received no samples under the INSACOG programme at all.
Mishra worried that states with plateauing COVID-19 cases aren’t realising the importance of starting their sequencing programmes during this lull, instead of waiting for spikes. Sequencing is most helpful when it is widespread and prospective, like the UK’s programme that INSACOG is modelled after.
“That is how England was able to take some action with B.1.1.7,” Mishra said. “The more you sequence, the earlier you pick up the variant, and the more likely you are to preempt spread. It’s a simple equation.”
Several states don’t seem to have got the memo. There is also disagreement between INSACOG labs and the NCDC on who will chase after these samples. While the NCDC’s Singh said it’s up to each INSACOG lab to follow up on pending samples, officials at more than one INSACOG lab told The Wire Science that they couldn’t be held responsible for this.
Lack of motivation to sequence isn’t the only problem holding back states, however. There are also genuine logistical challenges – among them, the difficulty in ferrying samples at below -20º C across the country, and INSACOG’s exclusive reliance on RT-PCR tests at a time several states are doing too few of them.
For example, Rajesh Bhaskar, Punjab’s nodal officer for COVID-19, said his team has struggled to arrange for a courier service to transport samples at the required temperature to INSACOG labs in Delhi. Meanwhile, Utkarsh Betodkar, an official of the IDSP in Goa, said only one medical institution in the state was administering RT-PCR tests, and the remaining banked on antigen tests [footnote] A rapid test that detects proteins on the viral surface instead of viral genetic material like RT-PCR[/footnote] or a molecular test called TrueNat, which also detects viral genetic material like RT-PCR.
But since the NCDC had only called for RT-PCR samples, it was difficult to meet targets, Betodkar said. Another official from Uttar Pradesh, who didn’t want to be named, told The Wire Science that 60% of tests in the state were antigen-based, which didn’t leave enough samples for sequencing. And of the remaining, many samples didn’t have a sufficiently low cycle threshold.
These problems aren’t insurmountable, several scientists said. For one, avoiding sequencing antigen samples and RT-PCR samples with low viral loads altogether is a bad idea because it would create a selection bias, Divya Tej Sowpati, a scientist at CCMB, said. A few RT-PCR samples with low viral loads should also be sequenced even though sequencing failures would be higher, he added. Mishra said that if some towns or cities are using only antigen tests, they must be made to store samples too, for sequencing later.
But INSACOG hasn’t begun ironing out such details in earnest; its labs are foremost in need of the expected Rs 100 crore. The Wire Science asked Renu Swarup, secretary at the Department of Biotechnology, about the hold-up but received no answer.
The way forward

Given the formidable challenges in INSACOG’s way, did the consortium over-commit itself with its 5% goal? After all, until December, India was sequencing far fewer than 1% of its cases, and even a jump up to 1% or 2% would have been a useful improvement.
But scientists across INSACOG told The Wire Science that the 5% goal was not unachievable – especially given the current size of India’s outbreak. In January 2021, India reported 4,72,317 new cases, which means the consortium would have had to sequence 23,615 samples to hit its goal. The total capacity of the ten consortium labs, according to INSACOG’s guideline document, is higher than this: 27,800 samples per month.
And even if India experienced a surge, the labs can expand their capacity further, according to IGIB’s Agarwal. As of today, IGIB can sequence roughly 1,500 samples every four days – with a process to increase it to 1,500 samples a day, by automating the lab’s sequencing machines. “The current numbers we are seeing in India are nothing for us, if we decide to go full pace. The rate-limiting factor is not our ability to sequence but whether samples can get to us in time.”
All this is possible if labs are also not hobbled by irrational rules that slow them, said Mishra. The finance ministry’s goal to encourage Indian manufacturers was an important one, in his telling: India must eventually develop local capacity to make high-quality reagents and plastics for sequencing, instead of importing forever. The problem lies with the ministry’s decision to change rules overnight, in the middle of the pandemic. “They should have taken a graded approach, such as asking labs to reduce the use of imported goods over five years. If you ban everything in a day, we will be ill-prepared.”
But he is hopeful that with public health at stake, the government will help INSACOG labs by easing restrictions – and quickly. This is crucial because while new variants pose a grave danger in the coming days, the general population may be too fatigued to comply with strict measures like lockdowns.
“We have to ensure that if a new variant emerges – and they will emerge – they are picked up early and constrained. Otherwise, with the level of fatigue all around, we won’t be able to handle them,” he warned.
Note: This article was updated at 6:44 pm on February 28, 2021, to describe lab studies of viruses more accurately.
The reporting for this article was supported by a grant from the Thakur Family Foundation. The foundation did not exercise any editorial control over the contents of the article.
Priyanka Pulla is a science writer.

