
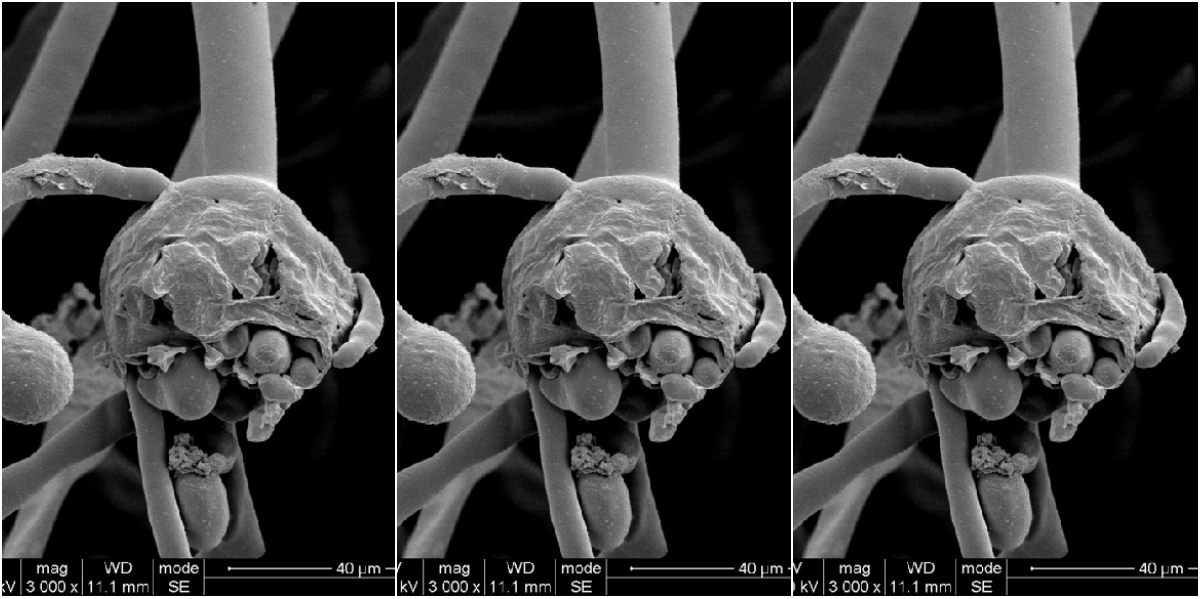
Candida albicans visualised using scanning electron microscopy (performed at CenSE, IISc Bengaluru). Image: Vader1941/Wikimedia Commons, CC BY-SA 4.0
India has been reporting a growing number of instances in which people with or are recovering from COVID-19 are contracting fungal infections.
In many cases, healthcare workers have also reported that both black fungi (order Mucorales) and white fungi (Candida albicans) have shown resistance to multiple drugs and antifungal agents.
Worldwide, a class of compounds called azoles is predominantly used as an antifungal drug against both black and white fungi. And even before the COVID-19 pandemic, India had a substantial burden of azole-resistant strains of black and white fungi.
An azole is a compound composed of five atoms arranged in a ring, at least one of which is nitrogen and at most three of the other four are carbon. Here are four examples:

White fungi have also been able to resist many other drugs.
Currently, healthcare workers use a drug called amphotericin B to treat black fungus infections in COVID-19 patients. As it happens, there is some evidence to suggest that both black and white fungi could also resist amphotericin B in some cases.
‘Drug resistance’ simply means that the fungi are able to resist the curative effects of certain drugs. They can thus keep growing and spreading even in the presence of these drugs. This means the fungi don’t only resist the drug – they also acquire more disease-spreading ability.
On June 10, Mankind Pharma launched a drug called posaconazole to treat black fungus. A few days earlier, Bajaj Healthcare Limited received the US Food and Drug Administration’s approval to manufacture and market posaconazole’s active pharmaceutical ingredients. Posaconazole belongs to a category of drugs called triazoles.
Unfortunately, antifungal drugs belonging to the azole group can’t fight the black fungus in many cases because of its ability to resist azoles.
It’s possible that the abundant use of azole as a fungicide in agriculture is responsible for this reality. Researchers wrote in one 2017 study:
… epidemiological research demonstrated an increasing prevalence of azole-resistant strains in Aspergillus fumigatus. The main resistance mechanism is a combination of alterations in the gene cyp51A. Surprisingly, this mutation is not only found in patients receiving long-term azole therapy for chronic aspergillosis but also in azole-naïve patients. This suggests an environmental route of resistance through the exposure of azole fungicides in agriculture.
Also read: Explainer: Why Is Multi-Drug Resistance a Problem?
Azole-based fungicides are used to protect rice crops. And since the azole group (picturised above) is very stable, it can remain chemically unchanged in food and soil for many months. The uncontrolled use of azoles can render different species of fungi resistant to the whole azole group, as well as contaminate the soil, air and our food.
Drug-resistant fungi are substantially more pathogenic (i.e. have more disease-causing ability).
Drug resistance is a form of evolution. Microbes like fungi grow, reproduce and adapt in the presence of drugs while incurring structural changes in their genes. Evolution selects for those changes that help the microbe survive better.
They can be in the form of a chemical change on a small point of the genetic material, resulting in a point mutation. Or they can be much larger – such as one less or more chromosome, i.e. an aneuploidy. Some strains of Candida albicans have become able to resist echinocandin after undergoing both point mutation and aneuploidy.
Such genetic changes can stay on in fungi even when the drugs are absent.
Drug-resistant fungi are present in our environment. For example, azole-resistant Aspergillus fungi live in the soil. Their powdery black spores, through which they reproduce, disseminate in the air blowing around us. We can inadvertently inhale those spores.
They won’t cause disease right away, however. Instead, they are opportunistic: they wait for an opportunity to infect. This is why they are more harmful among immunocompromised individuals – such as COVID-19 patients.
Timely diagnosis of such fungal infections is important, including through specific diagnostic assays. RT-PCR tests can also help detect the presence of drug-resistant strains of fungi. Delayed diagnosis causes death in 88% of cases.
India’s current treatment guidelines don’t provide a robust evidence-based recommendation to treat black and white fungi. So it is important that we retain the medical records of both survivors and those who have succumbed to track the presence and evolution of drug-resistant strains in the population. Understanding the precise mechanism of resistance will also help guide the use of appropriate drugs.
Drug resistance can be a substantial burden on health infrastructure as well as turn into a global threat.
Madhurima Pattanayak is a freelancer science writer from Kolkata.

